Well the run up to Christmas has started and I hope you're enjoying your Advent Calendars (let's not pretend we don't still have them). I'm going to give you a rundown of the National Dementia Forum and some of the exciting ideas that I came across that are being put forward at a national level.
The event was held at the Royal National Hotel in London and the first item on the agenda was how much dementia care has changed over the last 25 years. This was presented by Vic Rayner, who is the executive director of the National Care Forum
Vic looked at what was needed to make sure that the needs and provision of dementia care were met in the forthcoming years. The answer is that more needs to be done to provide leadership and invest in staff.
Vic then went on to look at dementia policy and the prime minister's dementia challenge, which to those that don't know is that by 2020, the UK is to be the leading country in the world for people with dementia, their carers and families to receive support in and also the best country in the world for dementia research. This is an admirable aim but can only be achieved by all services coming together to work holistically with communities and families. This where the role of Dementia Action Alliances comes to the forefront on how we perceive dementia and what we can do to educate people in how best to help someone with dementia and the way that dementia operates.
Vic then spoke about how active listening can help when communicating with someone with dementia. Those of you that attended my Dementia Friends Training Course will already be familiar with this, but for those that didn't this is to do with the way that body language and posture can play a big part in the way that we communicate with someone with dementia. Giving the person time to respond and establishing their preferred method of communication is paramount to promoting effective communication and can greatly reduce the number of negative outcome incidents associated with dementia.
Vic then discussed the issues if equality for people with dementia that might be experiencing issues around poverty, sexuality, race, age, gender and health. This was quite relevant given the changes in the law and people's attitudes over the past 30 years; and the way that someone with advancing dementia might feel fear being in one of these groups given some of the prejudices that existed back then. It is important that when faced with someone with dementia that is experiencing these fears, that we acknowledge that the fear is very real before offering reassurance. That way the person with dementia feels listened to and will help in building trust between the person with dementia and the carer/family member.
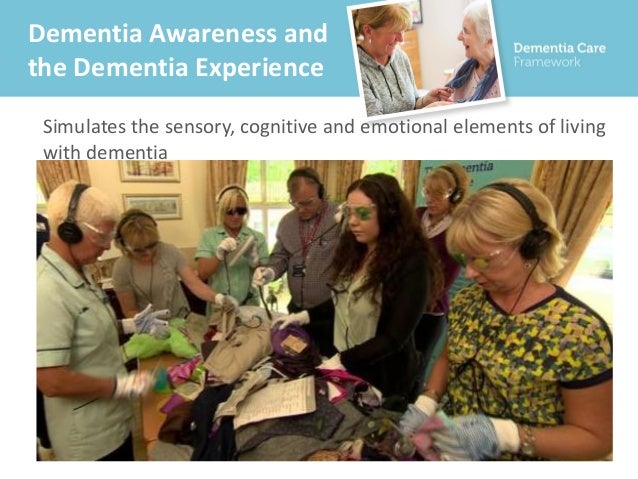
Vic then looked at how we can transfer power into communities to get feedback and offer solutions to the very real problems that they are facing when having to cope with dementia related issues. This again focused on the work that Dementia Action Alliances provide alongside useful meeting places such as Dementia Cafes and Carers Associations to discuss shared experiences and common problems. Alzheimer's Society and Age UK are dedicated to providing information and help for people that wish to know more on the subject and are useful allies in the dissemination of information required to realise the Prime Minister's Dementia Challenge. This tied in nicely with Vic's next point of how we train staff in the care sector to promote person centred approaches to service users and also how we can educate family members to help them cope better with some of the many challenges that looking after someone with dementia might face. We explored some of the technology available in helping with dementia from 3D interactive experiences through to the use of something as simple as a twiddle-muff.
The final part of Vic's presentation focused on some of the benefits of good nutrition in the diet of someone with dementia. There has been studies to show that good nutrition can slow down the advancement of dementia. Food such as fish, steak and green vegetables are rich in Omega 3 and this can help promote good brain function. Other sources of good nutrition included coconut oil, soya beans and the use of turmeric in cooking.
The next presentation was by Dr Karen Harrison-Dening, Head of Research and Evaluation at Dementia UK and this covered end of life palliative care in the field of dementia.
Karen identified that over 700,000 people in the UK have a form of dementia and that 30% of people over the age of 60 will die from or with dementia.
Alzheimer's disease is the biggest killer of women over the age of 60 at 13.4%.
The sad truth is that people with dementia, particularly those in the advanced stages tend to receive poor end of life care and this needs to change. Conversely it is rare that someone with dementia will receive hospice or palliative care as the disease is not perceived as a terminal illness. This means that a lot of the spiritual needs that someone would expect in end of life care are not being met.
The report also highlighted a failure of stakeholders to work together alongside a poor knowledge surrounding dementia by GP's as causes as to why people with dementia are experiencing poor levels of care.
In 2013, Dementia UK commissioned a report into the Future of Hospice Care to include those with non-malignant diseases, such as dementia. They also looked at special interest groups such as Admiral Nursing to improve dementia services and provide support and knowledge to other services.
This was split into five categories:
1. Generating Ideas.
2. Discussion
3. Further generation of ideas.
4. Discussion and generation of themes.
5. Ranking/Prioritisation.
Of the 15 themes generated in total the top 5 were:
1. Communication - this looked at not just communicating with a person with dementia during a distressed episode and recognising that everyone is different but also communicating with the person with dementia's carer also.
2. Pain Assessment and Management - this included how to understand assessing and managing pain, pain management for distressed behaviours and pain education which highlighted not just seeing and treating agitation.
3. Understanding issues for care in different settings - this explored having a shared ethos between hospices and care homes and looked at staffing levels within dementia care.
4. Education of the wider team (cascade) - this looked at sharing ideas and experiences between the different care settings
5. How to influence local policy and strategy - this looed at ways of getting management and clinical commissioning groups on board, making a case for people with dementia to access hospice care and dementia to be thought about and funded as seriously as cancer.
The outcome of this was to increase the number of Community of Practice (CoP) meetings per annum, plans to develop a website to share information and develop ideas. Develop an evaluation plan to measure the output of the CoP and to develop interest in the CoP from other areas and countries.
There have been 3 CoP meetings already in 2016, there are 180 members, 3 publications and 1 conference abstract submission.
The next speaker was Dr Clare Royston of Four Seasons Health Care.

Clare spoke of a new approach to dementia care that promoted a set of values and actions to support special resident experiences. Their ethos is to improve the lives of their residents and the communities that they serve by delivering specialist residential experiences and by being the best place to work in the sector.
Four Seasons base their practice around the individual experience and operate a find and fix approach to their service delivery. This incorporates the capturing of live information via iPads. This results in 10,000 pieces of information captured every month which is affecting the resolution time of issues from 12 to 5 days and is increasing customer satisfaction. This is all developed alongside current national guidelines and best practice.
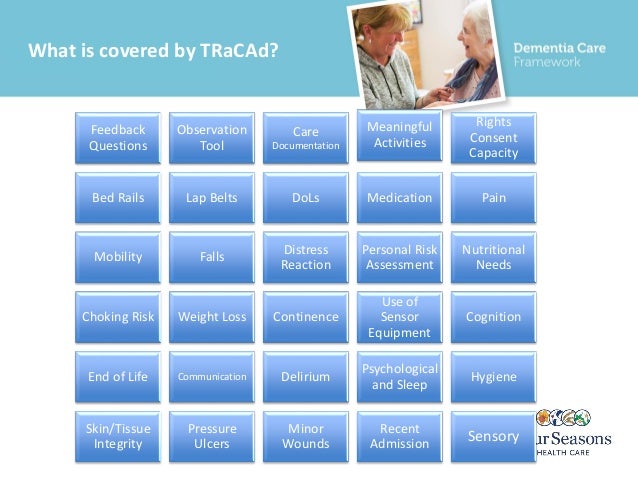
This is the screen that care providers and residents will use to log any issues in these areas. Staff are trained in using these devices and passing this expertise on to the resident population. By focusing on the needs of the individual, this is addressing more pertinent issues than traditional broad based training. Four Seasons also use the sensory experience to help staff understand the issues surrounding dementia and the frustrations that can be felt by a person with dementia.
Four Seasons also launched a Resident's and Families Charter. This looks at what is important to a resident and their families to produce a charter that connects directly to the way that the team delivers care. This is then linked into the Resident Experience Statements to look at the outcomes that have been produced.
The Residents Charter has 5 principles, which are:
1. Use what you learn about me to support me.
2. Call me by the name I know and prefer.
3. Listen to my wishes, preferences and concerns and support me to have my say.
4. Understand how I want to be cared for and if you have to make decisions for me, you strive to include me in doing what is best for me.
5. Help me to communicate with others.
The Families Charter also has 5 principles, which are:
1. Help me understand any changes in my relative's health and wellbeing and the care provided.
2. Listen to my thoughts and acknowledge and act upon any concerns and suggestions I may have.
3. Say sorry and put it right if you don't get it right.
4. Engage with me so that you fully understand my relative's personality, background, hobbies, likes and dislikes.
5. Support me to keep my emotional connection with my relative and spend quality time together.
The next presentation was carried out by Andrea Harman, a concept developer in healthcare for Saint Gobain Echophon which looked at the effect that noise has on a person with dementia.
This looked at what noise is and started with an exercise where different pitches were played around the room and dependent on your age, you could either hear the noise or not.
The description of noise is that it is an unwanted sound and that sound is a form of energy. Noise is also recognised as a source of stress and can cause a physiological reaction in the body. It also is shown that one can suffer a psychological reaction. It has an impact on intellectual performances such as writing and logical functioning. It is a major disruptor of sleep patterns.
Quiet, on the other hand, is recognised as one of the physical aspects of comfort.
As we age, we lose our high frequency hearing and become more sensitive to other frequencies of sound. Low frequency sounds are often linked to annoyance, aggression and fear. This can be anything from lorries to thunder to drums to factory/machine noise.
We struggle to hear what is being said in a noisy environment and this can lead to problems with communication. We can usually pick out consonants but vowels tend to be lost. This is because consonants contain the information in speech.
Of all the senses, hearing is the one that has the most significant impact on the quality of life for a person with dementia. A noisy or reverberant environment can be extremely uncomfortable for a person with dementia and can prevent good communication.
Difficulties in hearing, remembering and communicating contribute to the person with dementia engaging with their environment and people in it and can lead to social isolation. High noise levels in the living rooms of care homes were associated with low behavioural signs of social interaction. It has been shown that good room acoustics can make a real difference.
Things that affect room acoustics can be anything from shape, size, surface finishes and furnishings. Dementia friendly acoustics should consider where clear speech is important and where noise needs to be reduced or absorbed. Provide areas where people with dementia can seek respite if necessary. It has been shown that corridor noise is often a source of problems.
Positive sounds for people with dementia are often things that are found in nature. These can be things such as birdsong, flowing water and light rain. Music can also provide a positive sound for people with dementia, especially songs from the person with dementia's youth.
There is a strong case for adding sound absorption to rooms within a dementia care facility. Studies have shown that where acoustics are poor, people with dementia can be confused as to where the noise is coming from, have difficulty in engaging in conversations and were being disturbed by the noise reaching their bedrooms. When sound absorption was added, the people with dementia were observed to be far more settled, were engaging in more conversations and were having more settled sleep patterns.
The next presentation was carried out by Carole Henderson, who is the manager of Grief Recovery UK. This covered the area of grief in dementia care and why this is often overlooked in relation to dementia care. This was mainly about addressing the elephant in the room and focused on ways to explore the subject of grief. To find out more follow the link provided www.griefrecovery.co.uk
The next presentation was by Martin Neal, a lecturer in mental health and dementia studies from the University of Bradford. Martin looked at anger issues surrounding dementia and how to work with them.
Martin explored how anger is often a situation that carer's and relatives view to be problematic and a challenge to themselves and how to reframe this so that we could look at the repertoire of interventions that could be used to work with anger.
LOWLINE takes the approach that anger may not always be bad, that it can be an indication of an unmet need, that it can be part of a grieving process and that it can be a manifestation of fear.
What LOWLINE is not is a way to avoid managing angry individuals, a way of keeping people calm, an advanced high level intervention requiring lots of training and not just for professionals and staff.
LOWLINE looks at the benefits of active listening and reading non verbal cues and using positive body language to make a person with dementia feel listened to.
We then looked at validation theory and the works of Kitwood and Fiel, that espouse person centred approach to dementia care. Fiel looks at all behaviours having meaning and the responsibility of the person interacting with the individual to identify the meaning of the behaviours.
We then looked at The VIPS model :
. V A value base that asserts the absolute value of all human lives, regardless of age or cognitive ability
. I An Individualised approach based on uniqueness.
. P Understanding the world from the Perspective of the person with dementia.
. S Positive Social psychology in which the person living with dementia can experience relative well-being.
We also looked at Blackwell's Model that uses the acronym VERA to establish it's approach. VERA stands for :
V = Validation
E = Emotion
R = Reassure
A = Activity
This again concentrates on putting the individual first when dealing with any behavioural responses that are associated with anger.
The next presentation was given by Catriona Sudlow of the Dementia Swimming Project
Catriona spoke about the potential benefits of swimming for someone with dementia. This included the value of swimming for improving insight into motivations, barriers and perceptions. Building partnerships between leisure, health and social care sectors and creating a network of dementia friendly pools.
Some of the recognised benefits of swimming include the relief of pain, independence, empowerment and social connection.
The group aims to increase dementia awareness among leisure providers. They also aim to make the service accessible, safe and supported. They carry out their own market research by getting feedback from people with dementia about their experiences in the swimming pool. They have also looked at barriers such as transport and in some area have linked in with local councils to combat this by forming transport partnerships.
To create a dementia friendly environment in the pool they have looked at things such as noise, signage, reflective surfaces, potential slip hazards, accessible changing areas and colour and contrast.
There was then some personalised testimonies from carers and people with dementia about how much the project had benefitted them.
The next presentation was by Dr Vasilki Orgeta regarding depression in people with Early stage dementia.
This focused on the concept of IDEA (Intervention to prevent Depressive symptoms in EArly stage dementia).
People with dementia are at increased risk of depressive symptoms or depression. The presentation considered current research in the area and the development of a psychological intervention based on behavioural activation to prevent depression in people with early-stage dementia.
The theory is to schedule activities to obtain positive reinforcement, using the activity as a pleasurable experience (reward). After consultation with people with dementia, carers, home managers and relatives, the results were that being active stimulates the mind and body, that being active gives structure to the week, improves self-esteem, gives you a purpose and helps in staying calm. It helps in coping with loss and can ward off depression and loneliness.
There was then a presentation by Julia Pitkin a Dementia Coach and trainer.
Julia presented a video of the relationship between a son and his mother. The mother was a person with dementia. The first scenario outlined the mother looking for her purse and when she could not find it, blaming the son. This had a detrimental effect on the relationship, as the son could not cope with what he perceived to be an irrational attack on him, as the mother began accusing him of stealing her money.
The session then consisted of explaining validation theory, whereby the person with dementia has their feelings acknowledged and empathetic listening is employed. In relation to the scenario, this included taking on board that the person with dementia was feeling angry because she couldn't find her purse and validating their feelings. This included making statements such as I can understand that you're angry, should we contact the bank, would you like me to help you. This helped the person to calm and then address the situation.
We then cut back to the video, where the son employed this process and it displayed how the person with dementia could then explain their feelings and the relationship was able to be rebuilt.
The next presentation was given by Aileen Jackson, a Senior Project Manager for the South London Health Innovation Network.
This presentation consisted of a paper based framework that has been developed by the South London Health Innovation Network.to help care workers identify people with dementia.
The final presentation was given by Luke Tanner, an Associate Trainer at Dementia Care Matters.

Luke started the presentation by asking what we thought of as home and the feelings associated with it.
The feelings that were explored were peacefulness, being settled, being calm, contentment, safety, security, belonging, capability, comfort, happiness, confidence, freedom and ability. It looked at home as being a place, a person or a thing that makes you feel at home in yourself.
Luke then explored some of Kitwood's theory regarding what makes a person with dementia feel valued such as comfort, inclusion, attachment, occupation and identity that culminates in a feeling of being loved. This links in to your feeling of well-being.
Luke then looked at the psychological and behavioural symptoms of dementia. This included screaming, restlessness, physical aggression, agitation, wandering, anti-social behaviour, cursing, shadowing, anxiety, depression, withdrawal, hallucinations, delusions and psychosis. We looked at how relationships affect all of these in relation as to how to regulate stress.
We then looked at how people interact, especially in relation to staff and residents. We discussed emotional intelligence and how to be responsive to people's needs and feelings. We discussed where staff could interact more and eat with people at meal times to build up more natural relationships.
We looked at the removal of uniforms and getting rid of the them and us attitude that can sometimes permeate throughout the care sector. There was discussion around 30 second conversations and 60 second activities and how this can help occupy someone with dementia.
There was then a very interesting discussion regarding clutter. As the dementia progresses having things in an orderly fashion may not be the best way for someone with dementia to access material. For example, if someone with dementia was to walk into a room and there was a set of books on a bookcase, then those books would stay there unread, whereas if a book was left open on a coffee table, the person with dementia would be more likely to nose through that book.
We then discussed challenging routine bound care by "being a butterfly". This looked at changing the moment, turning tasks into experiences, being spontaneous and going with the flow, going along with different realities, focusing more on social interaction, using stuff in interactions, staging activities rather than running them and being aware of controlling language and behaviours.
We then looked at matching care giving to the different stages of dementia. Foe someone at the early stages of dementia it was about focusing on opportunities for domestic activities and accessing small reminiscence groups. There was an onus on creating banter during care giving interactions and greater independence in daily living tasks.
For someone experiencing a different reality there was activities such as completing half finished tasks, rummaging through boxes of their own personal items. There was an opportunity for role play as the person experiencing a different reality could carry out tasks from previous jobs and roles that were part of their reality.
Finally we looked at those in the latter stages of dementia. This included holding comfort objects such as dolls or stuffed toys. This concentrated on a soothing approach to the individual and accessing as much sensory items and equipment as needed.
The main message was that if we make a home feel like the person with dementia's home, then we can deliver a higher quality of care that is person centred in approach.
And that was the forum ended. I hope you've enjoyed reading my recap of the day and I would like to wish all of you out there a very Merry Christmas and a happy and prosperous 2017.